Who does Health Access Connect serve and from where?
#Closingthedistance #Accesstohealthcare #healthforall #Joinus #donate
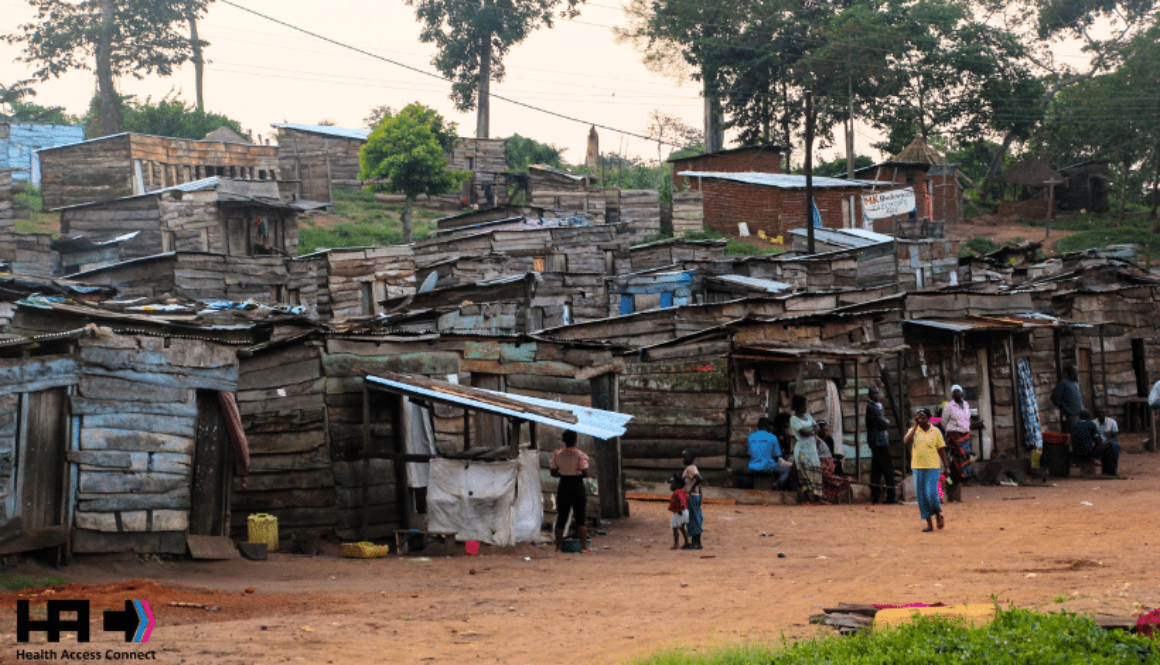
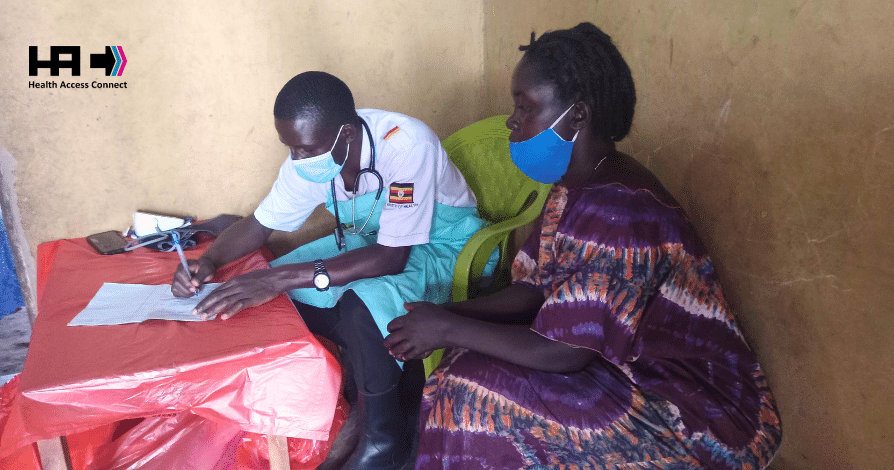
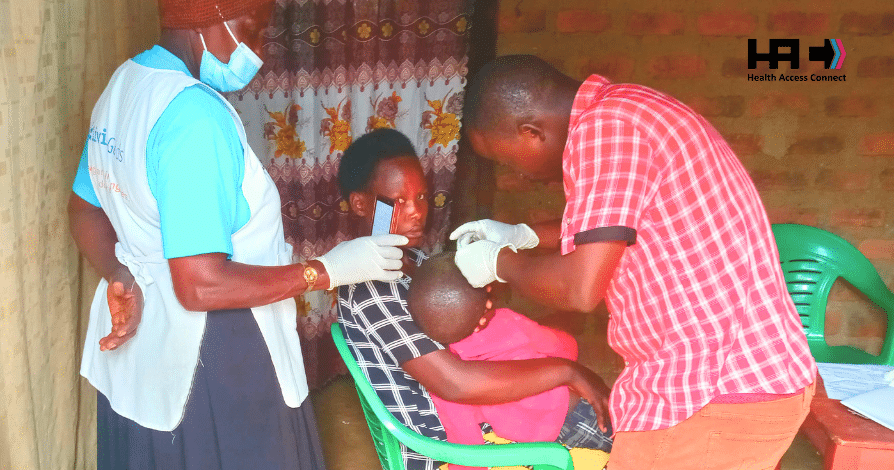
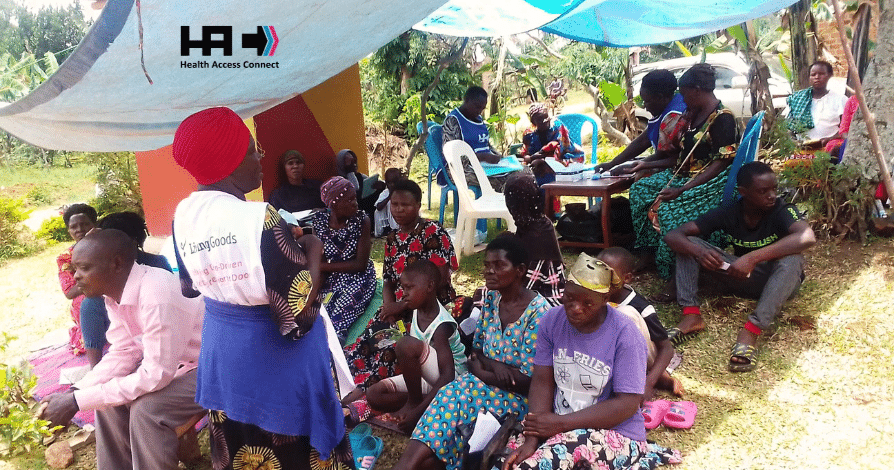
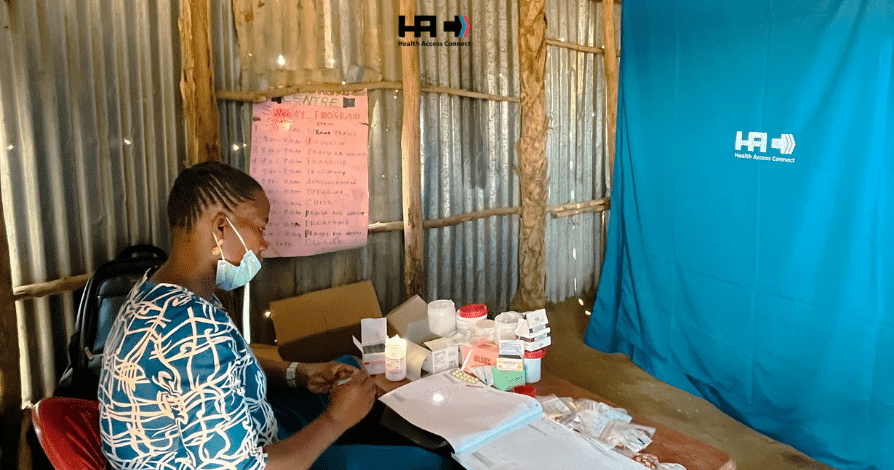
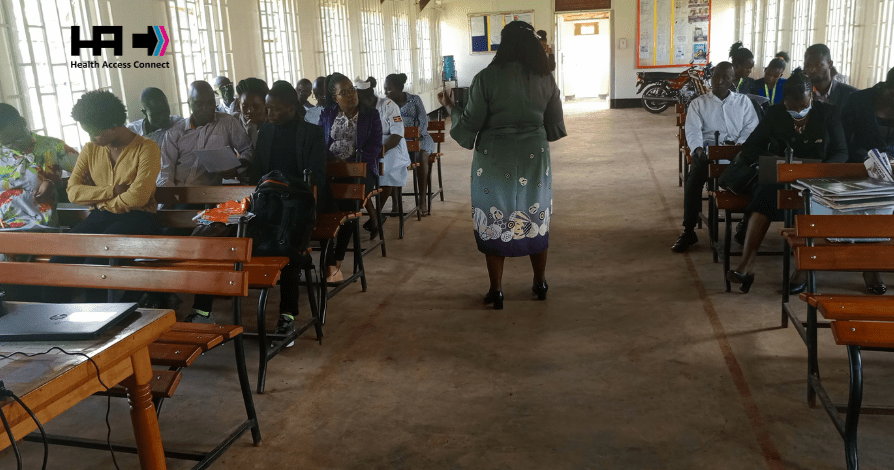
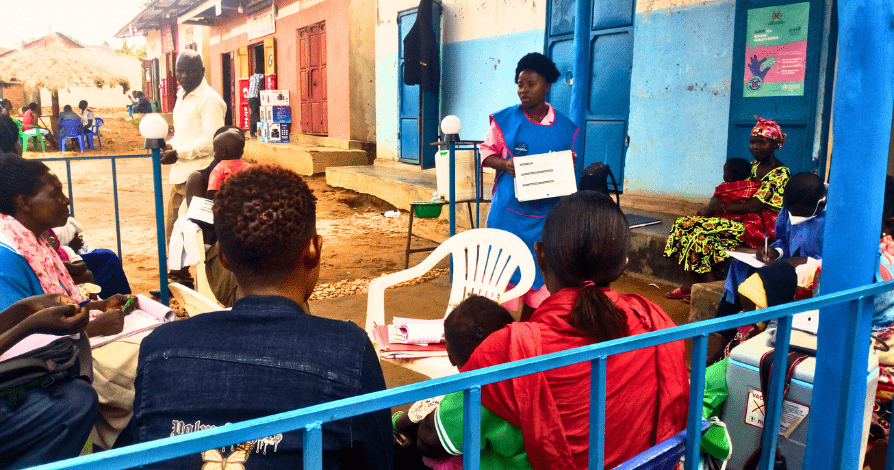
The heart of Health Access Connect’s mission lies in recognizing the unique characteristics of its target groups. Imagine a scenario where individuals must endure a journey of over four hours on foot to reach the nearest healthcare facility, or resort to expensive motorcycle or taxi rides, spending a significant portion of their meager daily earnings just to access medical care. These are the stark realities faced by the communities Health Access Connect aims to serve.

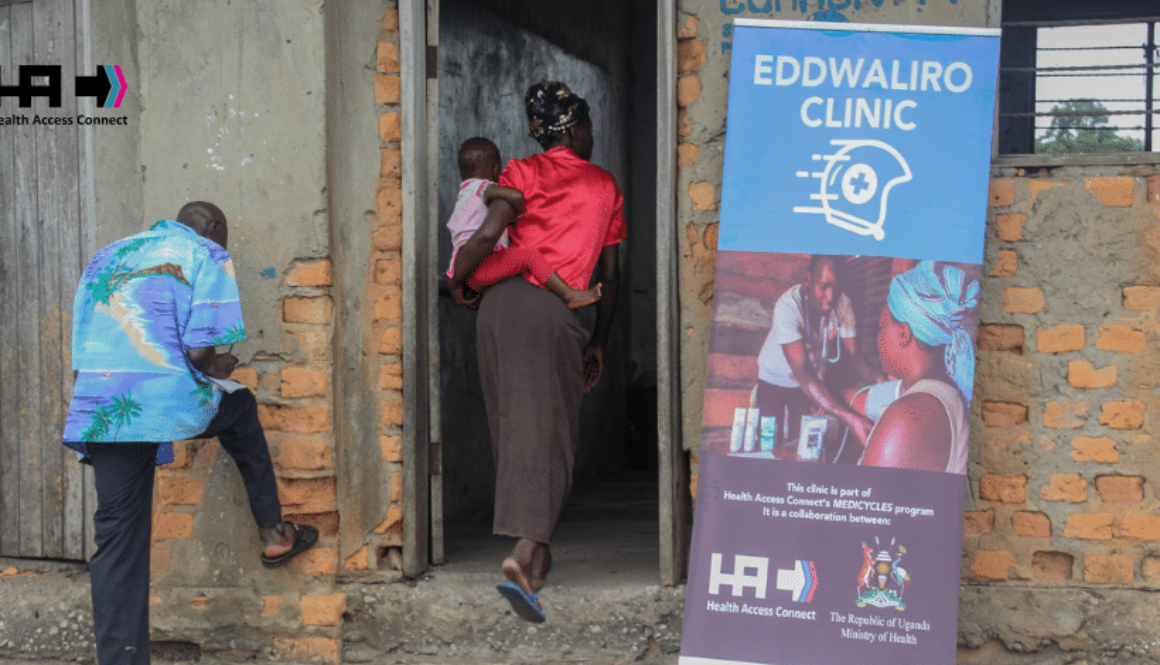
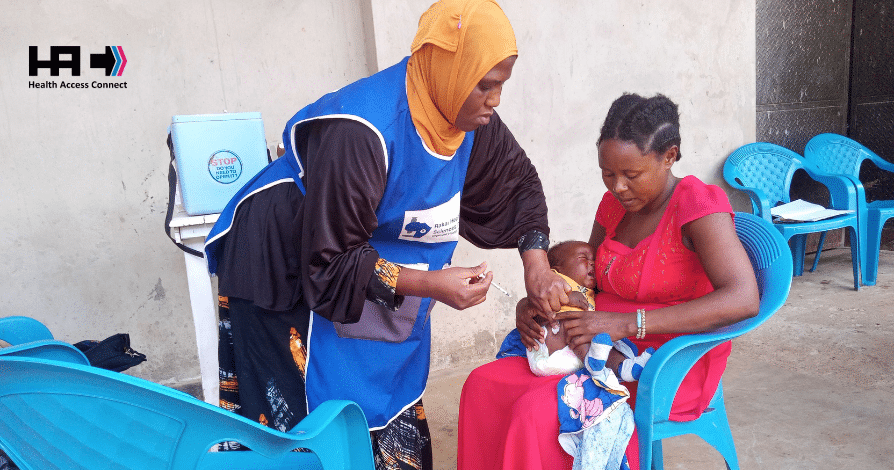
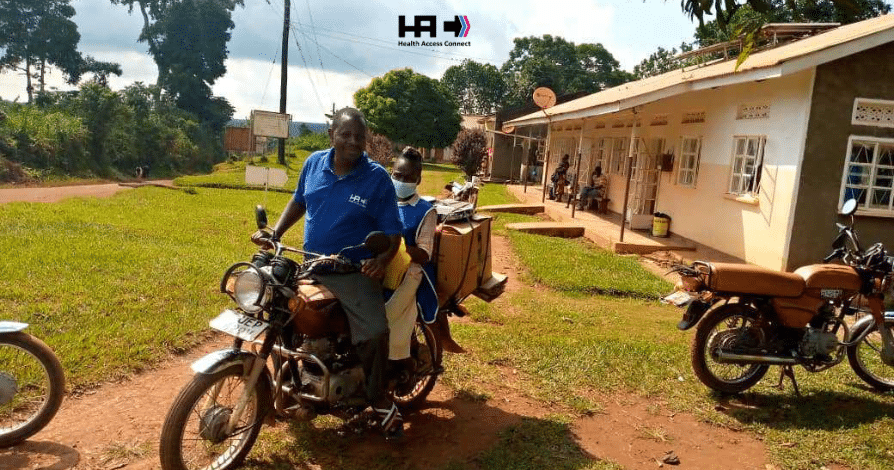
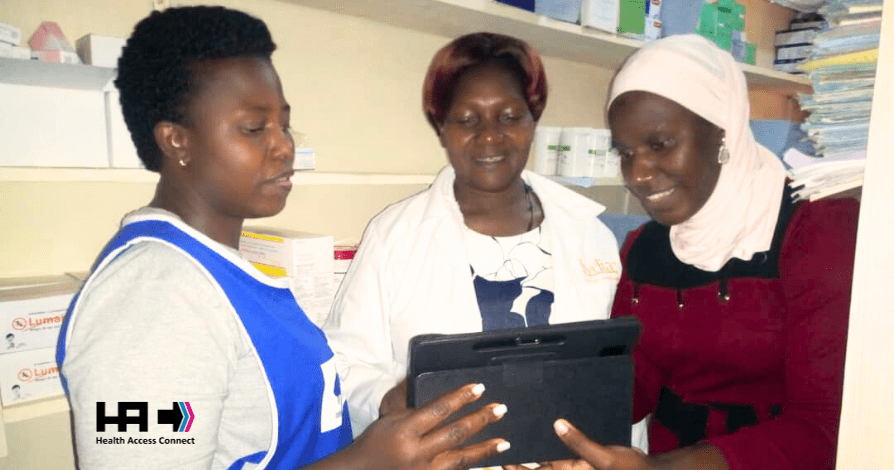
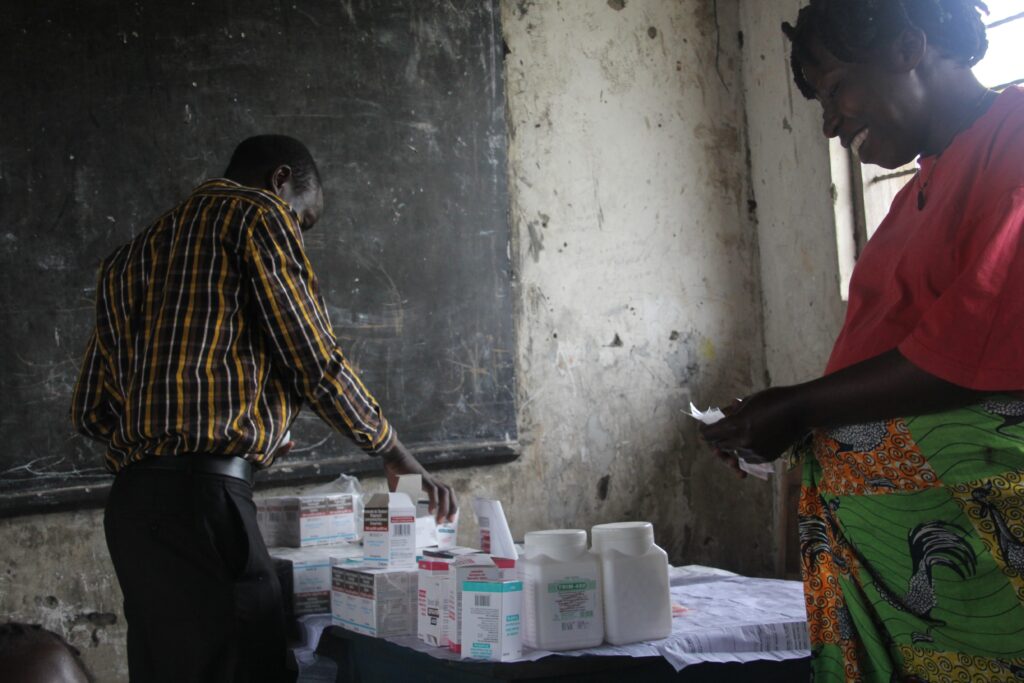
The story of Health Access Connect began with a profound realization of the dire circumstances faced by people living on the Islands of Lake Victoria. In these remote locations, individuals grappling with HIV were unable to access life-saving drugs available on the main island due to transportation challenges. In response to this pressing need, Health Access Connect introduced the Medicyle program – an innovative initiative that involved transporting government medical personnel via boats or motorcycles to various islands, thus ensuring that healthcare reached those in need.


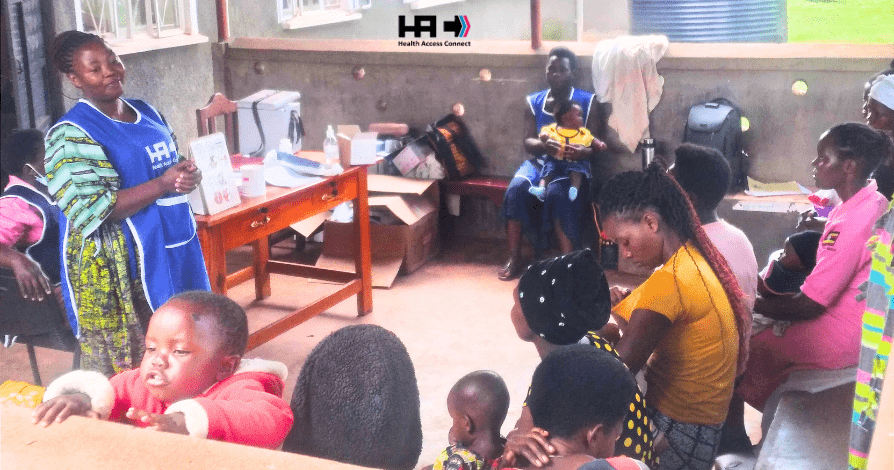
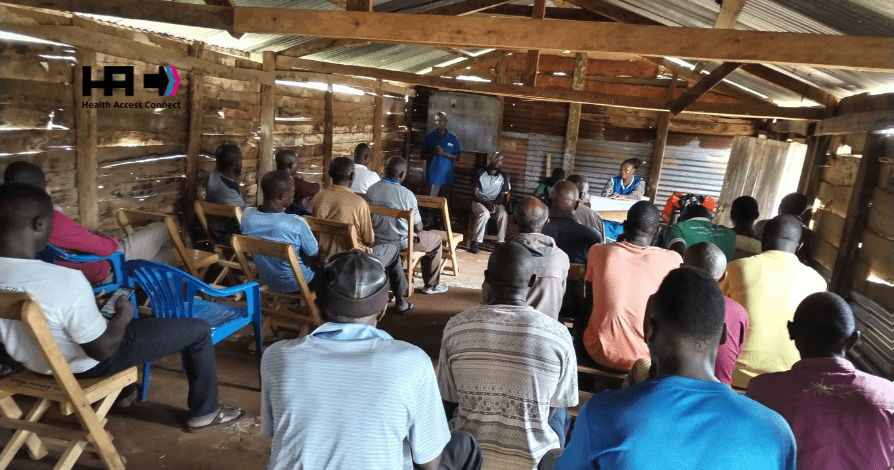
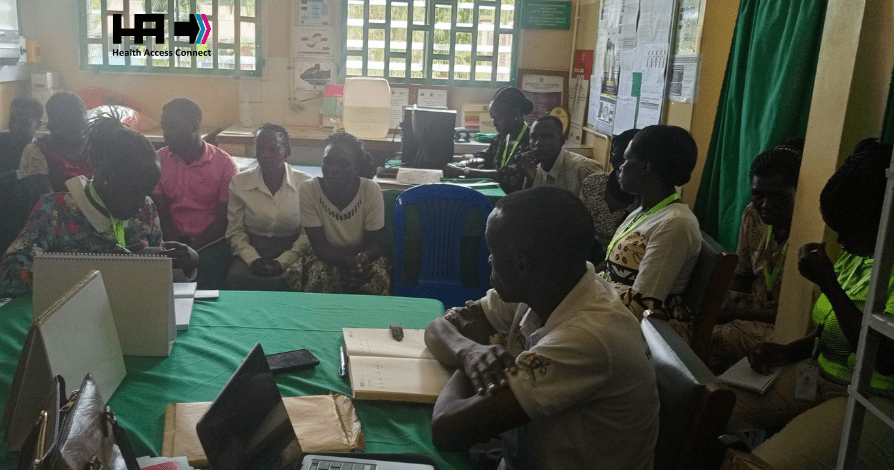
The success of the program in the Kalagala Islands prompted Health Access Connect to expand its reach. The same model proved effective in the fishing areas of Masaka, where HIV prevalence was a pressing concern. Today, Health Access Connect operates in 13 districts across Uganda, actively addressing the healthcare needs of communities facing geographic disadvantages and those residing 5 km away from the nearest facility.


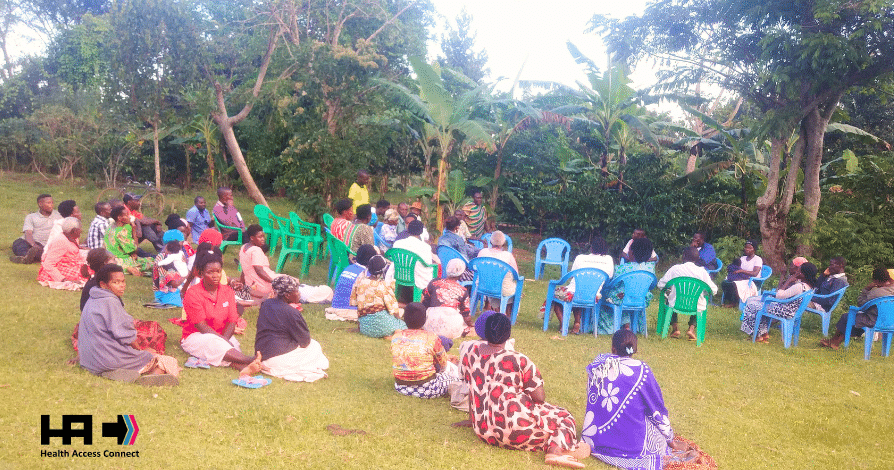
Geographical barriers should never dictate one’s access to healthcare. Health Access Connect firmly believes that every individual, regardless of their location, deserves access to medical care. This unwavering commitment has fueled the organization’s efforts to bridge the healthcare gap in remote and underserved communities.

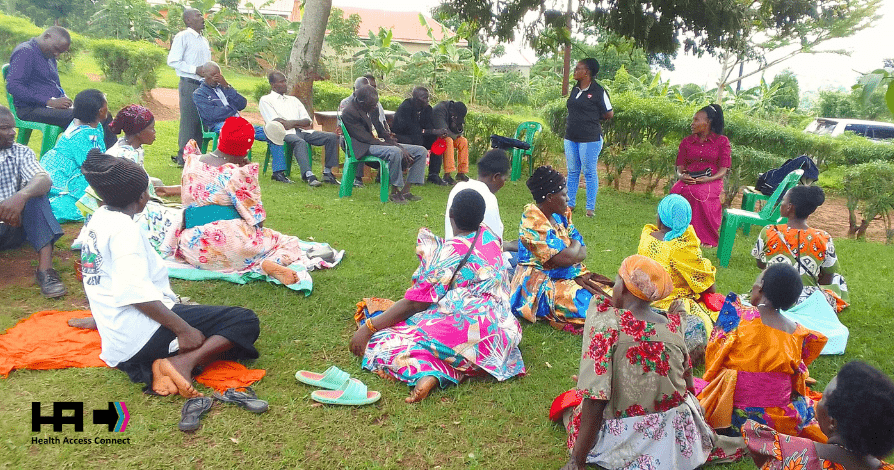
As Health Access Connect continues to make strides in reaching more communities, the call for support becomes even more crucial. The organization invites individuals, businesses, and institutions to join hands in ensuring that more underserved communities are connected to healthcare. Your support can make a significant difference in the lives of those who are currently facing the harsh realities of limited healthcare access.

In conclusion, Health Access Connect’s focus on geographically disadvantaged communities, fishing villages, and areas located 5 km away from medical facilities underscores its dedication to inclusivity in healthcare. The organization’s journey, from the Islands of Lake Victoria to 13 districts in Uganda, is a testament to the impact that targeted efforts can have on improving the health and well-being of underserved populations. As they express gratitude for serving over 120 communities, Health Access Connect looks forward to a future where healthcare is truly a right for everyone, regardless of their circumstances.